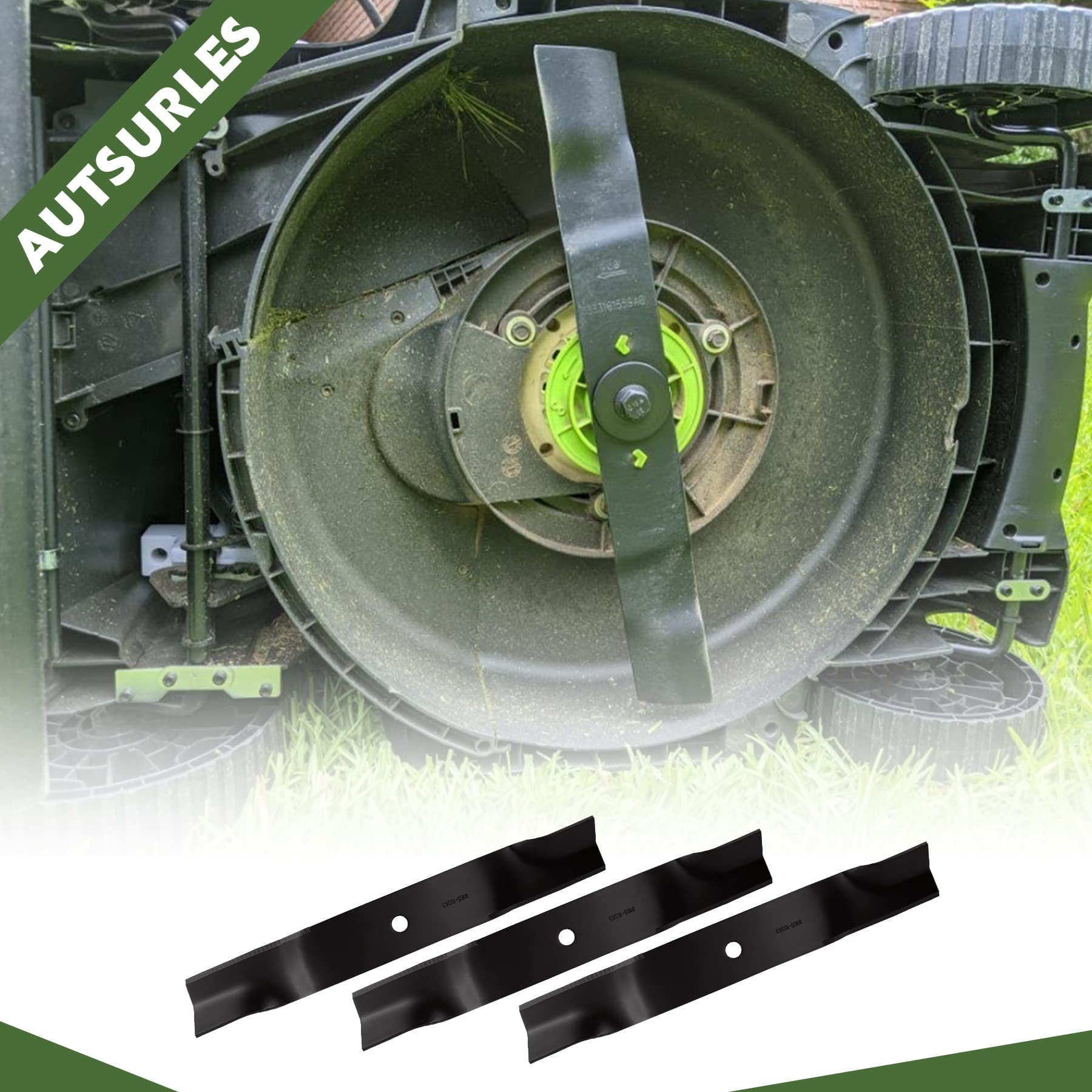
3 Lame Per Tagliaerba Cub Cadet - OEM, Taglio 60", Codici 02005019/1005338/942-04415, Per Modelli Recon M60
Disponibile
Disponibile
€ 21
AGGIUNGI AL CARRELLO
Consegna
- Corriere espressoda venerdì 13 marzoGRATIS
Venduto e spedito da ePRICE

Altri 14 venditori a partire da € 23
- Informazioni legali
- Ne hai uno da vendere?
- 1339319
- 17130197866
Pensati per Te
Prodotti simili
Descrizione
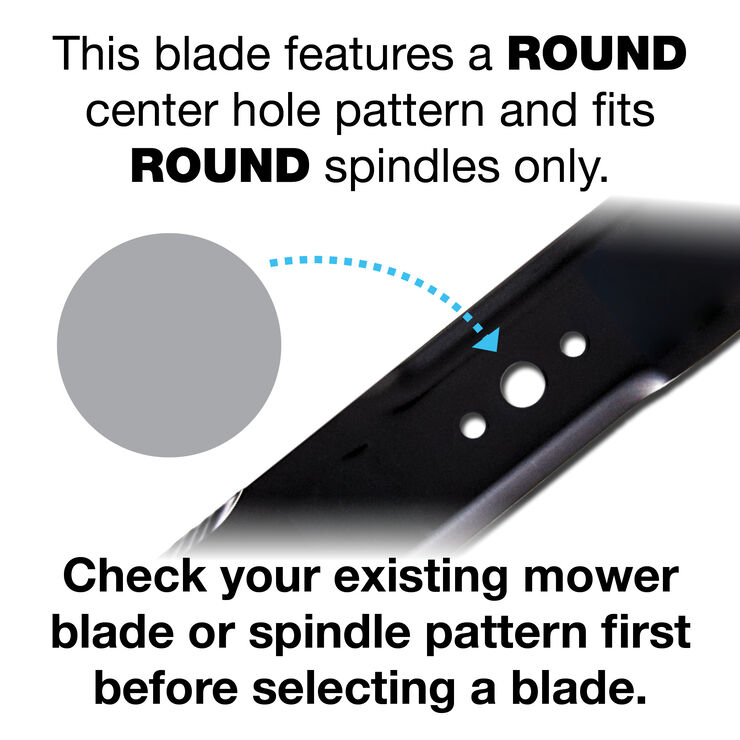
Se il tuo tagliaerba Cub Cadet non taglia più bene, queste lame OEM sono la soluzione! Set da 3, taglio 60\, codici compatibili 02005019, 1005338, 942-04415. Nuove, nella confezione originale, per modelli Recon M60. Ideali per manutenzione ordinaria o sostituzione stagionale. Facili da montare e bilanciate per prestazioni ottimali. Consegna rapida e qualità garantita. Tieni il prato perfetto con ricambi originali!Caratteristiche e scheda tecnica
Caratteristiche principali
- EAN4672037871883
Recensioni
2026-03-07 | muo0u8h