Set Paraluce In Gomma Pieghevole Con Fiore Tulipano 52mm + Panno Per Pulizia - Circuit City
- Corriere espressoda venerdì 27 febbraioGRATIS

- Informazioni legali
- Ne hai uno da vendere?
- 491272
- 77657850738
Pensati per Te
Prodotti simili
Descrizione
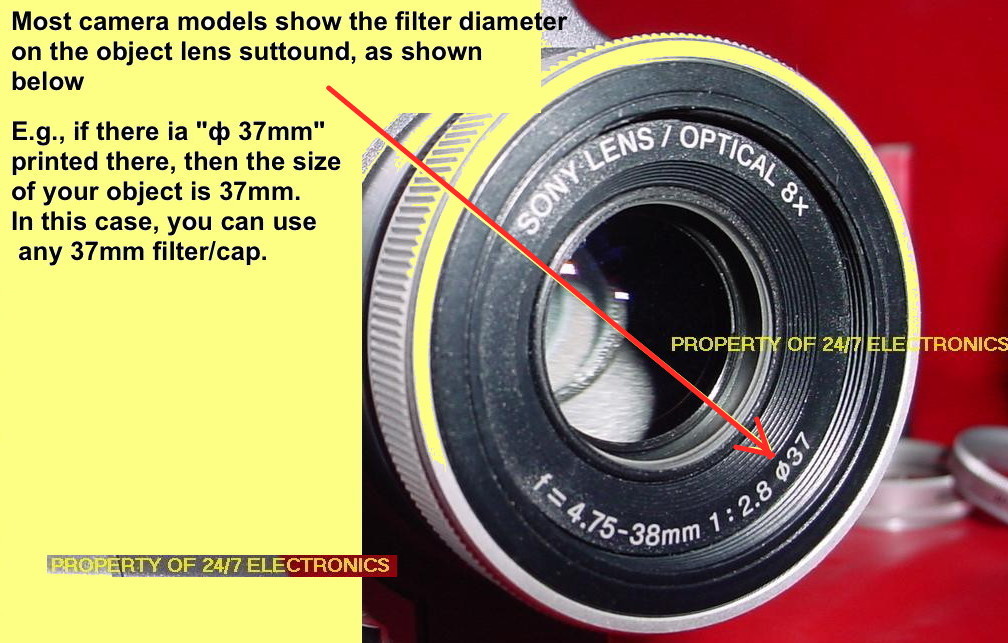
Vuoi proteggere le tue preziose lenti della fotocamera dai riflessi e dai raggi di luce parassiti, ma con un tocco di stile? Questo set di Circuit City è perfetto! Include un paraluce in gomma morbida e pieghevole con un grazioso motivo a fiore di tulipano, progettato per obiettivi con diametro filtro da 52 mm. La gomma lo rende facile da montare e da riporre, e si piega senza rompersi. In più, il kit include un comodo panno in microfibra per pulire delicatamente le lenti. Il codice MPN è GEN52MMPFLHK1, UPC 816129026889. Il prodotto è nuovo, nella confezione originale, con garanzia del produttore. Attenzione: include un avviso Prop 65 per la California. Ideale per fotografi amatoriali, viaggiatori o chi vuole proteggere l'obiettivo dello smartphone con un adattatore. Funzionale, originale e pratico. Dona un tocco personale alla tua attrezzatura fotografica e tieni le lenti al sicuro!
Caratteristiche e scheda tecnica
Caratteristiche principali
- EAN9835887084949