If you are a DMEPOS supplier and are purchasing opt-in Medicare leads, you should be aware of Medicare’s prohibition against telephone solicitation of beneficiaries.
In order to enroll as a Medicare DMEPOS supplier, and as a condition of payment, DMEPOS providers must meet various standards, including an agreement not to contact any Medicare beneficiary by telephone except under a few limited circumstances. 42 C.F.R. § 424.57(c)(11). The applicable exceptions are as follows:
- The individual has given written permission to the supplier to contact them by telephone concerning the furnishing of a Medicare-covered item that is to be rented or purchased.
- The supplier has furnished a Medicare-covered item to the individual and the supplier is contacting the individual to coordinate the delivery of the item.
- If the contact concerns the furnishing of a Medicare-covered item other than a covered item already furnished to the individual, the supplier has furnished at least one covered item to the individual during the 15-month period preceding the date on which the supplier makes such contact.
So, under this rule, unless the beneficiary is an existing/returning customer, the only time it is permissible for a DMEPOS supplier to contact a beneficiary by telephone is when that person has given the supplier “written permission” for such contact. But what does that mean, exactly?
Unfortunately, although perhaps not surprisingly, the rule does not define some key terms, including what it means by “written permission.” And as with so many issues, the rule has not kept up with advances in modern technology. For example, if a Medicare beneficiary “ops in” through an online advertisement by clicking a link expressing interest in being contacted about an item, does this satisfy the rule’s “written permission” requirement? The rule simply does not address this or any other such issues.
CMS has, however, released some non-binding guidance that, while not directly addressing the question above, might shed some light. One such guidance document is the “telemarketing frequently asked questions” document available on its website. While the FAQs do not address the question raised above, one of the FAQs could be argued to be somewhat relevant to the analysis:
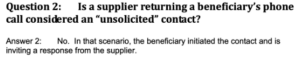
Although the supplier in the above-referenced hypothetical wouldn’t be returning the beneficiary’s call, one could argue that the same policy applies; the only real difference is the mode of the beneficiary’s opt-in.
Similarly, when it issued its final regulation in 2012, CMS responded to comments that had been sent in by interested stakeholders during the administrative “proposed rule and comment” process. One of the commenters suggested that the rule be amended to allow for beneficiaries to provide verbal consent to be contacted, in addition to written consent. CMS expressly rejected this suggestion, stating that “[d]ue to the potential for abuse, we believe it is important that there by a documented record of the beneficiary’s approval of the contact.” In light of this analysis, there is a good argument that so long as the supplier maintains evidence demonstrating that the beneficiary opted in via IP address, they have satisfied the spirit of CMS’ rule, if not the actual language.
To be clear, none of this should be read as advice that online opt-ins satisfy the “written permission” requirement. As has been made clear, there is no guidance directly on point. However, there is a strong argument that documentation proving that the beneficiary “opted in” by clicking a hyperlink and expressing interest in being contacted about an item satisfies this requirement. Accordingly, if you are purchasing opt-in leads, it would be advisable to maintain such documentation in the event of a later audit or investigation.
The attorneys at Chilivis Grubman represent DMEPOS suppliers and other healthcare providers and suppliers in connection with audits, investigations, and litigation. If you need assistance with such a matter, please contact us.
